From Uneven Beds to AI-Powered Care—India’s Healthcare Needs More Than Just Band-Aids to Heal Its Deepest Fault Lines
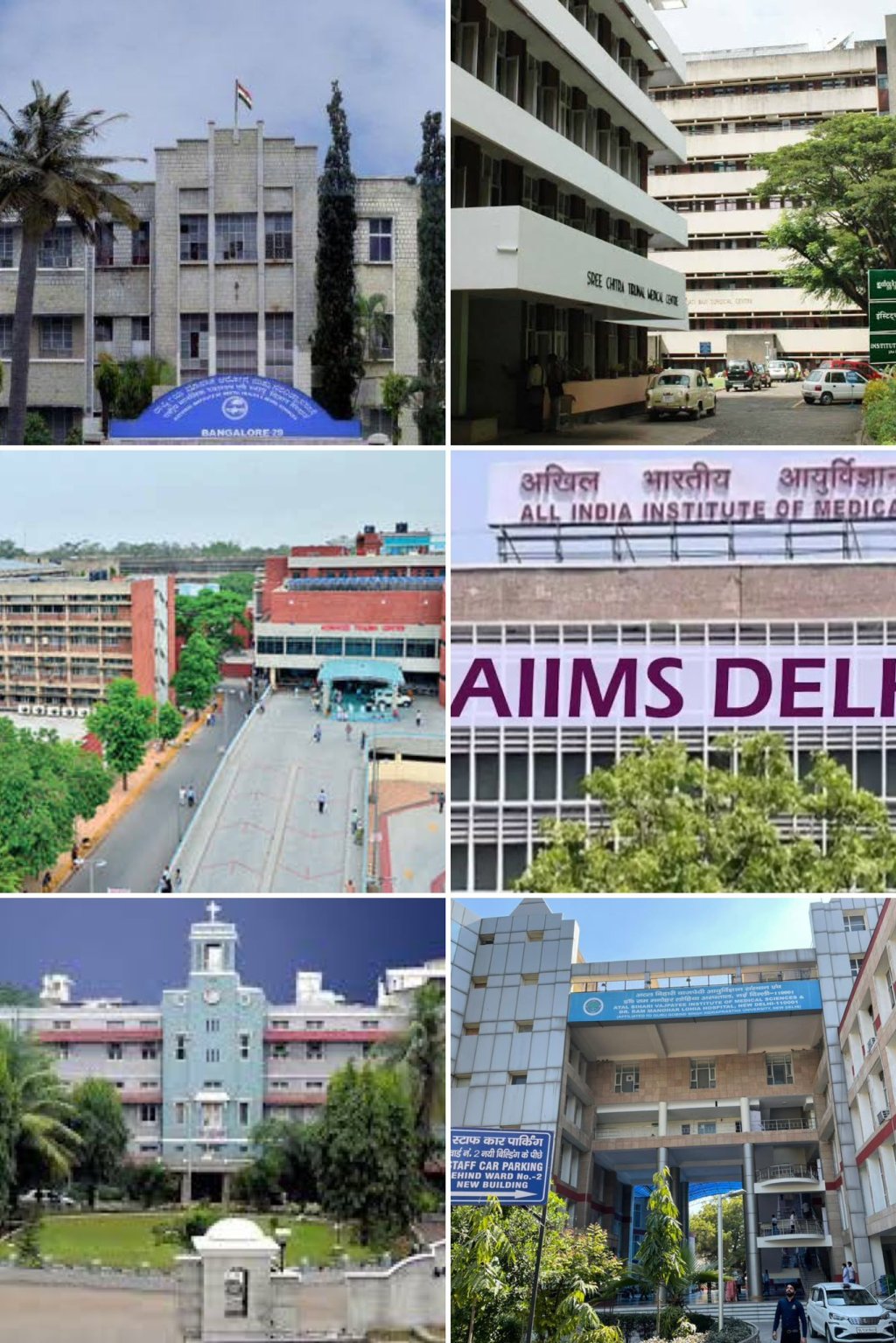
India’s hospital industry is navigating a moment of profound transformation, shaped by rising demand, evolving expectations, and persistent structural imbalances. As one of the world’s largest and most dynamic healthcare markets, it finds itself at the confluence of opportunity and adversity—where institutional scale must align with equitable access, and clinical ambition must coexist with operational realism.
Traditional financial indicators—revenue growth, margins, and profitability—offer only a partial view of the sector’s vitality. The underlying performance narrative is far more intricate, influenced by variables such as bed occupancy, case-mix complexity, patient turnover, technological integration, and clinical outcomes. Hospitals must constantly recalibrate their operational models to balance emergency care with elective procedures, adapt to shifting disease profiles, and deliver consistency across geographic regions.

In response, new institutional frameworks have emerged. Regional clustering strategies, hub-and-spoke models, and the expansion of specialized care centres have been deployed to maximize efficiency while deepening market presence. These approaches are indicative of an industry embracing complexity through strategic segmentation and infrastructure optimization.
Despite such progress, foundational asymmetries persist. Urban centres continue to attract disproportionate investment, while rural areas remain underserved—both in terms of medical infrastructure and human resources. This imbalance places mounting pressure on public hospitals, which face capacity constraints and outdated equipment, often serving as the last resort for large swathes of the population.

The financial architecture of the sector presents additional vulnerabilities. With health insurance penetration still modest, a majority of patients rely on out-of-pocket expenditure, exposing them to medical impoverishment and reducing the predictability of hospital revenue streams. Reimbursement delays under public schemes further erode cash flows, limiting the capacity of institutions—especially mid-sized providers—to invest in expansion, technology upgrades, or workforce training. The burden of rising input costs—ranging from medical consumables to energy and compliance overheads—only compounds this fragility.
On the regulatory front, the industry continues to operate in a landscape of fragmented licensing requirements, variable price controls, and limited transparency. While intended to improve patient protection, these mechanisms often deter private investment and restrict innovation. Compounding this is the absence of robust outcome-based reimbursement frameworks that could otherwise reward quality and efficiency.

Human capital remains a defining constraint. India’s doctor-to-patient ratio remains below WHO benchmarks, with wide inter-state disparities and a troubling rural-urban divide. Brain drain continues to siphon off highly trained professionals seeking better opportunities abroad, while the rapid pace of technological change necessitates constant upskilling of clinical and paramedical personnel—a task many institutions are ill-equipped to manage at scale.
Despite these challenges, a path forward is both necessary and feasible. The expansion of healthcare access must be underpinned by robust public-private partnerships and smart infrastructure deployment across underserved geographies. Financial models must evolve to expand insurance coverage, accelerate reimbursements, and reward performance rather than procedure volumes. Policy reforms should focus on regulatory simplification, data-driven accreditation systems, and pricing models that safeguard patient access while enabling provider sustainability.

Developing the healthcare workforce will require a fundamental rethinking of medical education, stronger incentives for rural placements, and widespread adoption of continuous professional development frameworks. Technology must also be fully integrated—not as a supplementary tool but as a core driver of efficiency, from AI-enabled diagnostics to secure digital health records and telemedicine platforms that bridge distance and expertise.
India’s hospital sector is slowly emerging from an era of uncoordinated growth and moving toward institutional maturity. This shift reflects a growing emphasis on clinical governance, operational accountability, and patient-centric models of care. In doing so, the sector signals its readiness to engage with the challenges of the next decade—not merely as a service provider, but as a foundational pillar of national development.

The future of Indian healthcare will not be shaped by protectionist instincts or episodic reforms. It will depend on strategic investments, cross-sectoral collaboration, and a cultural transformation that places health equity and clinical excellence at the centre of the policy and practice continuum. In rising to this challenge, India can craft not only a more resilient healthcare system—but also a more just and healthy society.
Visit arjasrikanth.in for more insights